Lung cancer surgery is an option for some patients depending on the type, location and stage of their lung cancer and other medical conditions. Attempts to cure lung cancer with the surgery involve removing the tumor along with some surrounding lung tissue and often lymph nodes in the region of the tumor. Removing the tumor with lung cancer surgery is considered the best option when the cancer is localized and unlikely to have spread. This includes early stage non-small cell lung cancers and carcinoid tumors.
What to Expect
Key Points
- Surgery is not an option for all lung cancer patients.
- Surgery involves removing part of or the entire lung.
- Prepare for surgery by watching the What to Expect video above and using this worksheet to stay organized.
How Is Lung Cancer Surgery Performed?
There are two commonly used approaches to removing portions of the lung. The choice depends on the location, size and stage of the lung tumor and the expertise of the surgeon.
- Thoracotomy
This is an incision on the side of the chest and follows the curve of your ribs. It typically involves dividing some of the muscles of the chest wall and uses an instrument to gently spread between two ribs to provide the surgeon access to the lung. The muscles are repaired when the incision is closed. - Minimally invasive surgery
This approach typically involves 1 to 4 small incisions to access the inside of the chest. The surgeon uses a camera to visualize the lung and special instruments to perform the surgery. This is known as thoracoscopy or video-assisted thoracoscopic surgery (VATS) and can also be done with the assistance of a surgical robot.
Types of Procedures
Possible Lung Cancer Surgery Side Effects
Each type of lung cancer treatment option has possible side effects.It is important to know the potential side effects and ways to cope with them before beginning lung cancer treatment. You might experience:
- Pain
- Possible complications from the lung cancer surgery
Discuss concerns, possible side effects and any effects that you experience with your surgeon. Download a list of suggested questions.
Reviewed and approved by the American Lung Association Scientific and Medical Editorial Review Panel.
Page last updated: November 17, 2022

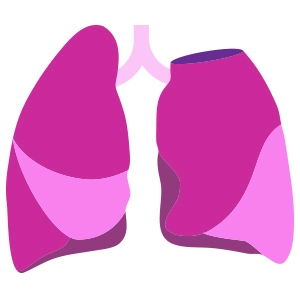
 The right lung is divided into three lobes; the left lung has two lobes.
The right lung is divided into three lobes; the left lung has two lobes.