Below, learn about immunotherapy in treating lung cancer, understand how it impacts patients and see how you can help immunotherapy research efforts.
New Hope for Lung Cancer Treatment
Dr. Mary Jo Fidler and lung cancer survivors, Karen and Donna, talk about the hope of lung cancer immunotherapy. There has been much progress in lung cancer immunotherapy. For the most up to date information, read our information below. In loving memory of our friend, Karen Loss.
Karen: It was right around Thanksgiving, I'd been having chest pains and I was afraid at one point I was even having a heart attack. So I went to have it checked out and my heart was okay, but they found something more serious.
Donna: In November of 2012, I had gone to the doctor to find out why I kept gaining weight. I assumed I had thyroid problems.
Karen: The phone rings, I answer and it's my doctor. And she says, "Karen, I've got some rough news for you. It looks like you've got lung cancer."
Donna: Please don't let it be lung cancer because that's not a good diagnosis. The doctor called and I probably only had about four months to live.
Karen: I did chemotherapy, I did some maintenance therapy, and I did some more chemotherapy, but during that time the tumors began to grow some more.
Donna: So I began chemotherapy and I responded poorly, and so the doctor took me off of the chemotherapy for a few weeks and the tumors really began to grow.
Karen: We talked about the options and decided that immunotherapy was a good possibility and decided that's exactly what we would do.
Donna: I could start in a clinical trial for immunotherapy. I thought about it for about three minutes, and chose to go into the clinical trial.
Mary Jo Fidler: Immunotherapy is a cancer treatment that is designed to help the patient's own body fight the cancer cells. The immune system is constantly surveying our body to see what doesn't belong. In particular, the immune system uses T cells to find and destroy cancer cells and viruses. The genes of the cancer cells are unstable and constantly changing, and that allows cancer cells to acquire new skills to avoid the immune system. One way it does this is through the development of the PDL1 protein, which can silence T cells that have been activated against the cancer.
The immunotherapy drugs that we have for lung cancer are given through the vein, usually through an I.V. What they are doing is blocking the interaction between the PDL1 protein and the activated T cells. This is supposed to release the brakes on the immune system and let the immune system do its job and kill the cancer cells.
For me, immunotherapy in lung cancer has been the most exciting treatment that I have seen in my career.
Donna: Immediately upon beginning the immunotherapy, my tumors stopped growing and have remained stable for three years and counting.
Karen: It's something that I think is worth talking to your doctor about, just to see if it might be right for you.
What You Need to Know About Lung Cancer Immunotherapy
From how it works to who is eligible to possible side effects, get answers to your questions about lung cancer immunotherapy.
Immunotherapy for cancer, sometimes called immuno-oncology, is a type of medicine that treats cancer using the body's own immune system. Your immune system protects you from harmful foreign agents like bacteria and viruses. When it is working well, it attacks what shouldn't be in your body. The immune system also has measures in place that keep it from attacking things that should be there like normal organs of the body. Cancer is a tricky problem for the immune system because cancer cells used to be normal organ cells, so they have some familiar features. But when cells convert to cancer, they acquire some new features that ideally should be recognized as foreign and labeled for immune destruction. Immunotherapy drugs for lung cancer help your body recognize the cancer as foreign and harmful so your body can fight it.
1. Immune checkpoint inhibitors
The most progress in immunotherapy for lung cancer has been made in immune checkpoint inhibitors. Immune checkpoints are molecules on the immune cells that can start or stop an immune response. The immune system uses these molecules to help determine what is normal and what should be attacked. Cancer cells sometimes trick the immune system by displaying these checkpoints to stop the body from attacking them. Immunotherapy drugs can prevent the immune system from getting tricked and helps stimulate a response against cancer cells.
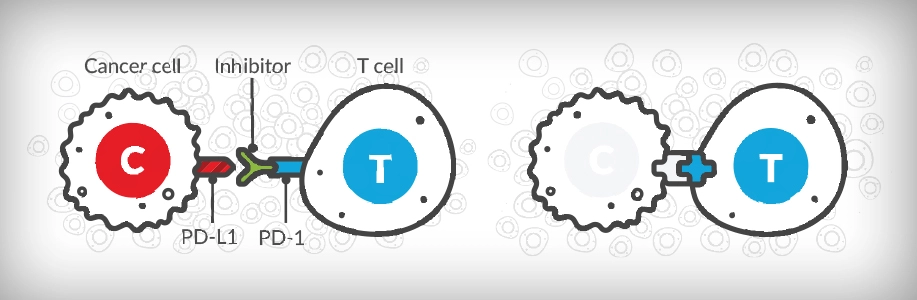
There are several drugs that target immune checkpoints that are approved for treatment of lung cancer. Many of these drugs block or "inhibit" the contact between the PD-L1 protein and the PD-1 receptor on the T cell. The PD-L1/PD-1 interaction functions as a brake that prevents the immune system from responding to cancer. By blocking this interaction, the immune system is able to recognize and attack cancer cells. One type of immune checkpoint inhibitor targets an immune checkpoint called CTLA4. When CTLA4 is blocked, the body is able to ramp up the number of immune cells that are available to respond against cancer cells.
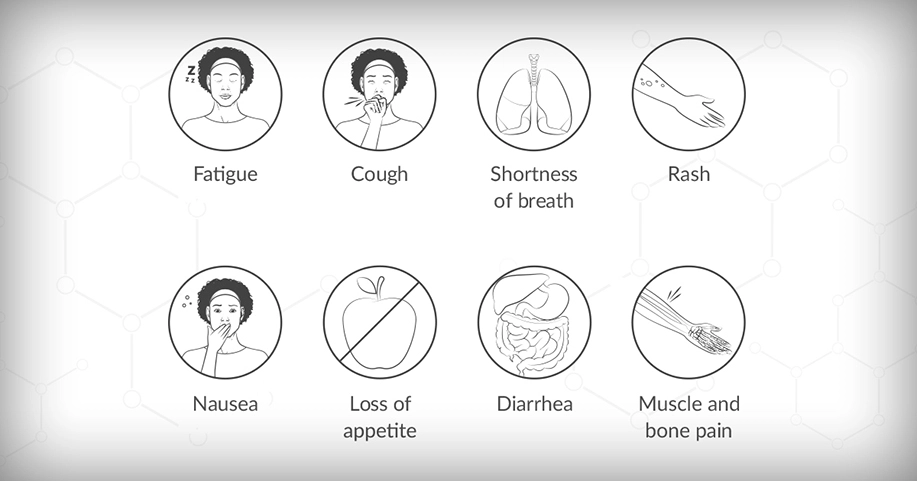
Checkpoint inhibitors are given as an intravenous (IV) infusion. These drugs can have similar side effects to chemotherapy, including fatigue, nausea, itching, skin rash, and more, but they are generally less toxic than chemotherapy. However, because the drugs work by stimulating the immune system, it is possible to develop serious immune-related side effects from an over-stimulated immune system that can affect how your organs function. It is important to work with your care team to help monitor all side effects.
2. Cancer vaccines
When most people think of vaccines they think of treatments that prevent disease. However, there is another type of vaccine called a therapeutic vaccine. This type of vaccine treats an existing cancer by making the immune system better at killing cancer cells. These vaccines target proteins that are present in cancer cells that are either not present in normal cells or are only sparingly present in normal cells. Sometimes, the vaccines are customized to target proteins that are unique to an individual’s cancer. In other cases, the vaccines target cancer-specific proteins. Before a vaccine is given, it is often necessary to first take a medicine to dampen the types of immune cells that may allow a cancer to grow and boost the types of immune cells that can respond to cancer. Right now, these vaccines are being studied in clinical trials. There is currently no FDA-approved vaccine for lung cancer treatment.
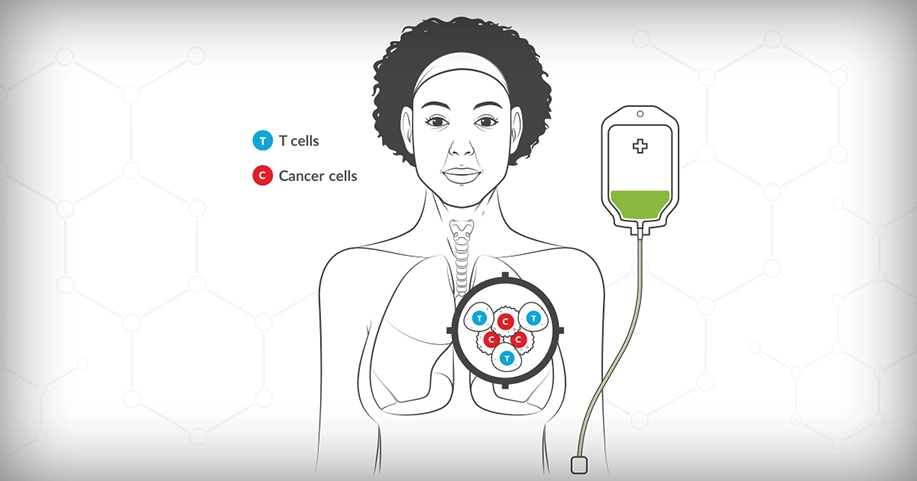
3. Adoptive T cell therapy
In this therapy, sometimes called CAR-T cell therapy, T cells, a type of white blood cell in the immune system, are removed from your body and altered in a laboratory so they are better at attacking your specific cancer cells. The enhanced T cells are then put back into your body to help it fight the cancer cells. Removing the T cells from your body can be done by a procedure called plasmapheresis, which helps filter your blood to specifically identify certain types of blood cells. Right now, this type of therapy is being studied in clinical trials and no such treatment is currently FDA-approved for treating lung cancer.
4. Bispecific T-cell Engager (BiTE®) Therapy
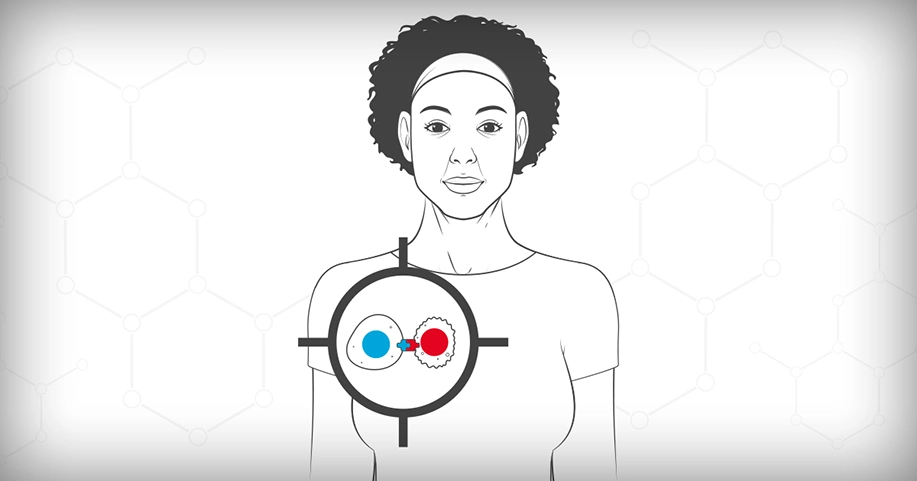
This type of immunotherapy is designed to bring a patient’s T cells closer to the tumor cells to help the immune system attack cancer cells that express a certain antigen (foreign protein) called DLL3. To do this, the medication which is given by IV, simultaneously binds a protein on the T cell called CD3 and the DLL3 protein on the cancer cells. Currently, this type of therapy is used to treat extensive-stage small cell lung cancer (SCLC).
There are several FDA-approved lung cancer immunotherapy drugs for patients with lung cancer. Many patients receive immunotherapy as the initial therapy for their cancer. Immunotherapy is sometimes given with chemotherapy. Sometimes, two different types of immunotherapies are given together. Each drug has specific indications (or uses) based upon on the type of lung cancer you have, whether you have any mutations or biomarkers, which treatment (if any) you have tried in the past and your general health. This information will dictate if you are eligible for immunotherapy and when you should receive it in your treatment journey. Work with your doctor to understand your options.
The immune system is made up of cells, tissues and organs that communicate with each other to protect the body. Your immune system uses different ways to communicate and gather information about whether to attack something it encounters or leave it alone.
One way your immune system communicates is through connections between molecules on the surface of immune cells (like T cells) and foreign cells (like cancer cells).
Cancer cells have found ways to trick the immune system to prevent it from destroying them. One way some cancer cells do this is by producing a protein called PD-L1 and placing it on the cell surface for T cells to "see." This protein binds to a receptor on the T cells called PD-1 which sends a message to the T-cell to not attack the cancer cell. The PD-1 receptor functions like a brake that prevents the immune system from killing the cancer cell.
Checkpoint inhibitor immunotherapy drugs work by disrupting the interaction between the PD-L1 protein on cancer cells and the PD-1 receptor on T-cells. When this connection is broken, T-cells are better able to recognize the cancer cells and respond to them. Drugs either target the PD-L1 protein (durvalumab, atezolizumab) or the PD-1 receptor (nivolumab, pembrolizumab). No matter which they target, they have the same goal of blocking or "inhibiting" the contact between the PD-L1 protein and the PD-1 receptor on the T cell. This re-activates the T cells and turns the immune system back on, helping it fight the cancer.
These drugs are given through an IV into your veins. This is called an infusion. Patients get infusions every few weeks. Most patients stay on immunotherapy for as long as their cancer responds to the immunotherapy. Some patients may stay on for longer or shorter periods of time, depending on their side effects. Immunotherapy drugs have been shown to keep working for a period of time even after treatment is stopped.
There are several FDA-approved lung cancer immunotherapy drugs for patients with lung cancer. There are more options within immunotherapy than ever before. Many patients with advanced-stage lung cancer receive immunotherapy as the initial therapy for their cancer. Immunotherapy is sometimes given with chemotherapy. Sometimes, two different types of immunotherapies are given together. Each drug has specific indications based upon the type of lung cancer you have, whether you have any mutations or biomarkers, what treatment (if any) you have tried in the past and your general health. Work with your doctor to understand your options.
Immunotherapy works differently than other lung cancer treatments like traditional chemotherapy, targeted therapy and radiation.
Traditional chemotherapy uses chemicals to kill or damage cancer cells. These drugs can affect healthy cells too. This can cause side effects like nausea, fatigue, hair loss, lowering of the white blood cell count, and possible infection.
Targeted therapy focuses on mutations or fusions that are in some lung cancer tumors. These therapies attack specific targets on or in the tumor cells that are causing the tumor to grow uncontrollably.
Radiation therapy uses powerful, high-energy X-rays or particles to kill cancer cells or keep tumors from growing.
Immunotherapy doesn't address mutations in tumors. Instead, it targets the communication between the immune system and the tumor to help the immune system fight the cancer.
You do not need to be in a clinical trial to receive an FDA-approved immunotherapy drug. However, there are promising lung cancer immunotherapy drugs currently in clinical trials. Participating in one of these trials might be the right treatment choice for you. Talk to your doctor about the clinical trials available to you.
All cancer treatments have possible side effects. When taking immunotherapy, some people experience very few side effects, while others have more serious complications. Some of the most common side effects of immunotherapy drugs are:
Immunotherapy may cause inflammation in the organs of the body. Inflammation can happen in any organ of the body including the lung (pneumonitis), liver (hepatitis), colon (colitis/diarrhea) or thyroid gland. This can be very serious, and all possible side effects should be discussed with your doctor before you begin the drug.
It is best to work very closely with your doctors and nurses to manage your side effects. Some side effects can be treated with over-the-counter medication. Other side effects may require prescription drugs or even time spent in the hospital. If side effects are managed early, it is easier to avoid major problems. If your side effects are well managed, it may also allow you to take only a short break or stay on the immunotherapy medication longer.
Ask about being connected with a palliative care team. Palliative care teams are made up of doctors, nurses and other healthcare professionals who are specially trained to help you manage your side effects and maintain a good quality of life.
Some patients have responded very well to immunotherapy, while others do not have the same positive response. No one can predict how your body will respond to any one treatment. Work with your doctor to understand what you can expect while on an immunotherapy drug, and if it is the right choice for you.
A procedure in which a machine is used to separate the plasma (the liquid part of the blood) from the blood cells.
Take Action
You can help advance immunotherapy research. Join the Lung Cancer Registry to help researchers learn from patients on immunotherapy.

Content supported by an educational grant from Merck.
Page last updated: January 21, 2026