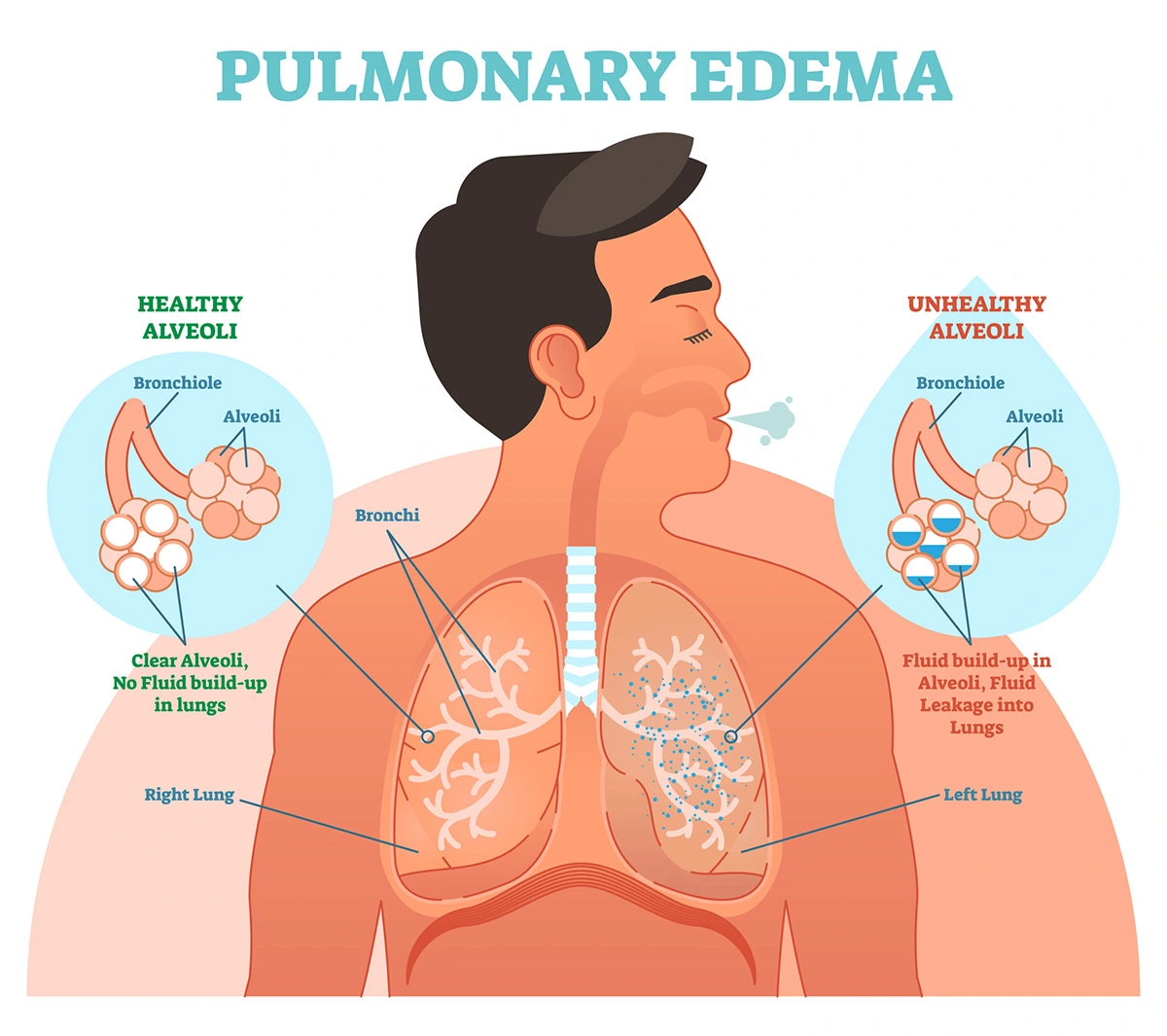
Edema is a fancy term for swelling caused by too much fluid. So, pulmonary edema refers to a condition where there is too much fluid in your lungs, making it hard to breathe. Specifically, fluid accumulates abnormally in the alveoli, or tiny air sacs, where gas exchange occurs. Under normal conditions, a delicate balance between fluid leaking from blood vessels into lung tissue and fluid removal via the lung’s lymphatic drainage keeps alveoli dry so oxygen can easily enter the bloodstream. When that balance is disrupted, fluid builds up and fills spaces that should stay air-filled. That fluid interferes with gas exchange, often impairing oxygen delivery to the body, which can lead to life-threatening breathing problems.
Jamie L. Garfield, M.D., a Professor of Thoracic Medicine and Surgery at the Temple Lung Center at Temple University Hospital in Philadelphia, sees this problem every day. “It is extraordinarily common,” she explained. “The good news is that most exacerbations can be avoided or intervened upon early before symptoms get severe.”
Causes and Signs of Pulmonary Edema
Though there are a variety of causes, pulmonary edema is generally classified as either cardiogenic (heart-related) or non-cardiogenic (not heart-related). Cardiogenic pulmonary edema is most commonly caused by congestive heart failure. When part of your heart stops pumping effectively, pressure builds up in the blood vessels of the lungs and forces fluid into the air sacs. Noncardiogenic pulmonary edema occurs when the blood vessels in your lung become damaged or "leaky” due to another disease, allowing fluid to escape into the lungs. Noncardiogenic causes include pneumonia, sepsis and trauma.
“Patients with pulmonary edema generally describe breathlessness. Sometimes they feel like they are suffocating or breathing underwater,” Dr. Garfield explained. In addition, the shortness of breath often worsens during movement or lying down, which may require them to be propped up on pillows to get some relief. Other symptoms include:
- Coughing up frothy, pinkish or bloody sputum
- Wheezing
- Chest pain or tightness
- Rapid breathing or heart rate
- Sweating
- Pale or bluish skin (cyanosis)
- Restlessness or anxiety
- Confusion or decreased alertness
Diagnosing and Treating Pulmonary Edema
Before your healthcare provider can diagnose and treat pulmonary edema, they will need to perform a physical exam, run lab tests and do imaging. Pulse oximetry can be used to assess oxygen levels. An X-ray is often the first imaging step because it can show fluid in the lungs, which can help rule out other causes of breathlessness. An echocardiogram, or an ultrasound of the heart, can check for abnormalities and evaluate the heart function. In severe or uncertain cases, invasive hemodynamic monitoring (e.g., with a pulmonary artery catheter) may be used to distinguish cardiogenic vs non-cardiogenic causes.
Treatment depends on the severity and the underlying cause. “Treatment for pulmonary edema is not difficult but the symptoms will not go away on their own without adjustments to medications and changes to diet,” Dr. Garfield explained. In emergencies, supplemental oxygen is essential and often the first line of treatment. Depending on severity, ventilators or respirators that directly deliver air into your windpipe may be needed. In many patients, diuretics, or water pills, can help remove excess fluid and ease pressure on the lungs. If the pulmonary edema is non-cardiogenic, antibiotics and steroids may be needed. If it is cardiogenic, medications to ease cardiac workload, improve heart function or manage blood pressure may be required.
In all cases, it is crucial to treat whatever triggered the edema to prevent recurrence. “It is important to remember that pulmonary edema is not a progressive disease but a treatable readily reversible condition with the right management.”
Pulmonary Edema vs. Pneumonia vs. Pleural Effusion — What’s the Difference?
Because fluid in or around the lungs can arise from different problems, it’s important to distinguish pulmonary edema from other lung conditions. Pulmonary edema, by definition, is a buildup of fluid inside the lungs, in the interstitial (tissue) and alveolar (air sac) spaces impairing oxygen exchange directly.
Pneumonia is primarily an infection of lung tissue caused by bacteria, viruses or fungi. In this case, the infection causes the lungs' air sacs (alveoli) to become inflamed and fill up with fluid or mucus which makes it hard for oxygen to get into your bloodstream. Because of this, imaging will pick up a dense, solid-appearing area in a lung lobe rather than a “flooding” of both lungs as in edema.
In contrast, pleural effusion occurs when fluid is collected in the pleural space or the thin layer between the lungs and the chest wall and not inside the lung tissue itself. A pleural effusion can compress the lungs from outside, but it does not flood the alveoli with fluid.
The suggested management and treatments differ greatly among these conditions, so correct diagnosis is critical.
Prevention and Considerations
Preventing pulmonary edema centers largely on managing underlying risk factors and conditions. For those at risk — especially people with heart disease, hypertension, valvular disease or chronic kidney problems — maintaining cardiovascular health is key. This means controlling blood pressure, avoiding salt and fluid overload, managing comorbidities, maintaining a healthy lifestyle and following medical advice closely.
“For example, patients who eat a lot of takeout are at high risk for exacerbating their heart failure and developing pulmonary edema,” Dr. Garfield continued. “Patients at risk for pulmonary edema need to understand the impact of processed foods and added salt on water retention, and they need to understand that blood pressure and heart rate control are paramount to keeping the heart in balance.”
Pulmonary edema can progress quickly to life-threatening respiratory failure, so if you are experiencing symptoms, it is crucial to seek medical attention immediately. Thankfully, if quickly identified and treatment, recovery is possible. Taking care of your heart and lungs, being cautious with altitude or strenuous water activities, and listening to your body — especially when breathing becomes difficult — are among your best defenses against a condition that, without treatment, can rapidly become life-threatening.
Blog last updated: January 12, 2026