As COVID-19 patients continue to flood hospitals and fill the Intensive Care Units (ICUs) with severe cases, many doctors are looking for new ways to save lives. One procedure that is beginning to get attention in the media is ECMO. Short for extracorporeal membrane oxygenation, also called extracorporeal life support or ECLS, ECMO is used as a temporary form of heart lung bypass in patients who have the most severe heart, lung or heart and lung failure.
But what exactly does the procedure entail and is it really the best course of action for patients with COVID-19? Dr. Erik Osborn, who specializes in pulmonary critical care medicine at Inova Health System and is the Medical Director for Adult ECMO, answered all our questions about this little-known procedure and its use during the pandemic.
“Historically, for about the last 40 years, ECMO has been used successfully in babies and children with severe lung failure or severe heart failure. Only in the last 10 years or so have we been able to demonstrate that it can be used successfully for adults with lung failure. Specifically, during the 2009 H1N1 pandemic, we found that ECMO could be used successfully in adults with the most severe lung failure. Since then, there have been well done clinical studies that support the use of ECMO.”
What is ECMO and how does it differ from ventilation?
Traditionally, lung failure is treated with mechanical ventilation, also called a breathing machine. These machines use positive pressure to push more air into the lungs and facilitate gas exchange, thus providing needed oxygen and removing carbon dioxide. The problem is that humans breathe naturally with a negative pressure breathing mechanism, so normally, when we inhale, the pressure in our lungs is negative, so breathing machines work the opposite of our normal breathing. For people who are very sick, this increase in positive pressure can strain the lungs by increasing the volume and pressure of air being inhaled, which in turn can cause lung injury. ECMO works because it allows the lungs to rest and it allows us to minimize the harm that the breathing machine causes.
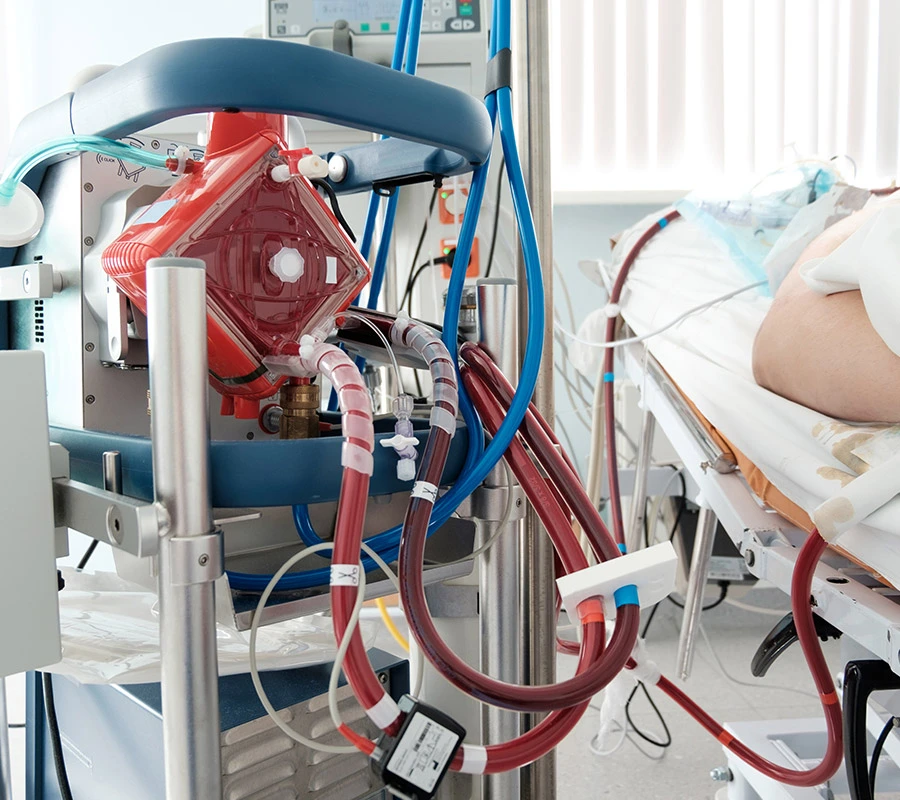
ECMO pulls your blood outside of the body from one large vein, puts it through a pump which then pushes the blood through a membrane lung that facilitates gas exchange externally. It then returns your oxygenated blood to your body via another large vein through a tube that's positioned close to the right side of the heart. The ECMO machine performs the function of the lungs successfully so the lungs can rest and we can use very low settings on the breathing machine. This protects the lungs from additional damage that the high pressures from the breathing machine cause.
Why is ECMO only used in certain situations?
ECMO is a complicated and specialized procedure that requires a special team that can manage the side effects and troubleshoot the machine itself. I think it's important for people to realize that it requires additional resources and it's a resource heavy system to operate. Optimally, a specialized ECMO team is necessary and that includes an ECMO physician, an ECMO Specialist, an ECMO advanced practice practitioner, an ECMO trained nurse and an ECMO trained respiratory therapist. There are multiple different team structures, but it requires a multi-disciplinary team to run ECMO successfully.
In addition, because of the influx of COVID-19 patients, our resources are strained. Across the country, we have all been limited by staff, equipment and even physical bed space. If you are going to put someone on a complicated machine, you want to make sure you have people that know how to take care of that machine as well as monitor the patient for any side-effects. There is a national shortage of nurses; so some places run out of nurses, then they may run out of ECMO machines, and finally they run out of actual beds. Over the last month, as expected, things have been getting worse.
The other challenge is that COVID-19 isn't the only disease that is putting people in the hospital. There are people with heart failure, pneumonia and multiple other causes of lung failure that could benefit from ECMO. So, we have our regular patients and then on top of that we are adding COVID-19 patients and many of the ICUs around the country literally don’t have enough staff or beds.
What are the side effects?
I'd say that one of the silver linings in the pandemic would be that the attention ECMO has received has highlighted the fact that ECMO can increase survival in a carefully selected group of patients. This is great but there's an important caveat to that, that ECMO is a complicated and specialized procedure which also comes with a significant set of side effects. They include bleeding, infection and organ failure, to name a few of the more common ones. This is why where it is done and the fact that it is performed by a specialized and experienced team with special training is so important.
What is the survival rate for ECMO patients?
I believe the most recent estimates for the survival rate for ECMO in the United States, for all types of COVID ECMO, is a little above 50%. Centers that do a lot of ECMO, however, may have survival rates above 70%. It's like anything else, if you go to a place that specializes in that area and has significant experience doing a particular complex procedure, then the survival is much better. This is why I think it is important for the public to understand that ECMO is a complicated procedure that should be done at specialized centers. It is also not a support system that will help everyone, it works best in carefully selected patients.
Like many procedures, ECMO works best when it's used early. The standard of care is that you use ECMO once the patients have failed the other evidence-based therapies. That includes lung protective settings on the breathing machine, so people have low volumes and low pressure on the ventilator. Then they also have to fail a trial of paralysis and they have to fail a trial of prone positioning (lying on their stomachs). You can do this all in one or two days, but if the patient is not improving, has low levels of oxygen or high levels of carbon dioxide in their blood based on a blood test, we evaluate them for ECMO.
The other point about the use of ECMO in a global pandemic is that choices about its use are similar to a combat medicine triage scenario. In a setting where you have limited resources, you want to use those limited resources on the patients who are more likely to survive. By doing this it allows us to save the largest number of lives, but that presents extremely challenging choices for healthcare providers to make.
To learn more about how COVID-19 is being treated, visit our COVID-19 Treatment and Recovery page.
Erik Osborn M.D., Medical Director for Adult ECMO at Inova Health System. He is a Pulmonary Critical Care Physician who recently retired as an Army Colonel after serving as an Army physician for 23 years. Dr. Osborn joined Inova Health System full time 2 years ago. Inova supported 121 patients with ECMO in 2020, and since the COVID-19 pandemic started the Inova ECMO Team has supported 52 COVID-19 patients with ECMO. Dr. Osborn has been teaching ECMO for Chest (American College of Chest Physicians) for over 10 years.
Blog last updated: October 10, 2023