We were so careful.
We wore masks before they were mandated. We sprayed all of our mail and washed all of our groceries. We stayed home. But by summer we heard the other arguments as well. Staying home was having an impact on kids/teens mental health. The virus could probably not survive on surfaces. It was safer to be outside and socially distant.
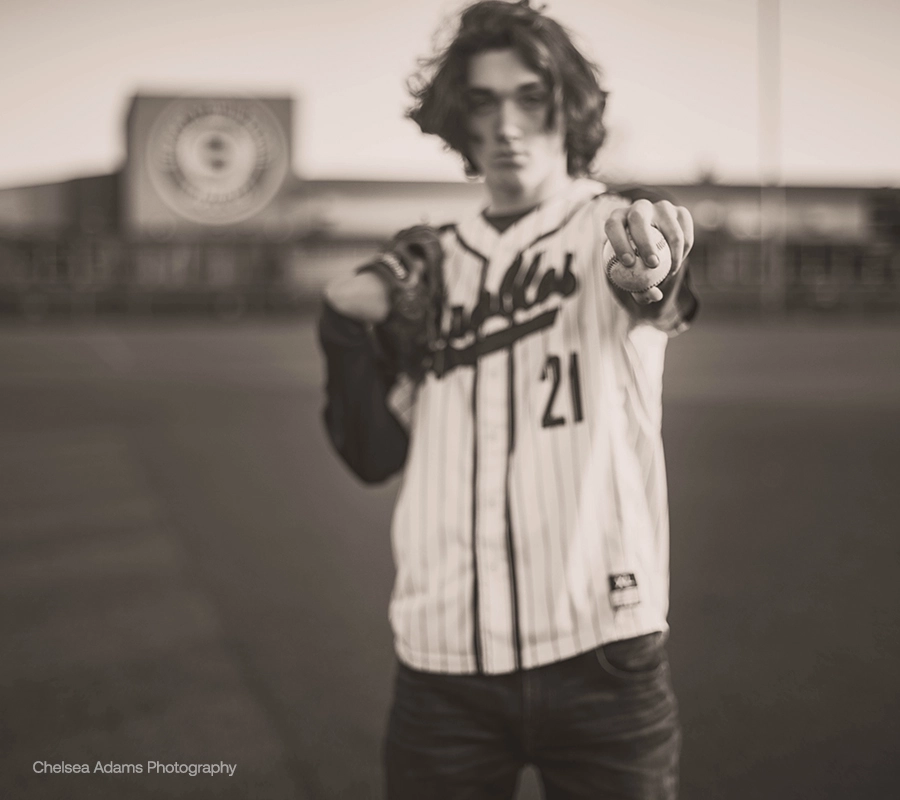
After three and a half months, we decided to take a calculated risk. We let our son start practicing with his club baseball team. After all, baseball is a low contact sport played outdoors. Carson is a 17-year-old pitcher. He spent all winter of his junior year in training, getting ready for the spring season. He is a 6’6” lefty and had dreams of playing baseball in college. COVID-19 hit and everything in Oregon shut down, just three days before he got the chance to play his first varsity game.
On July 7, Carson and his team played their first summer game. On July 9 we got a text from the coach that a sibling of a player tested positive, and that our games were on hold until the possibly infected player was tested. When his test came back positive, the entire team was advised to get tested. Carson started wearing a mask around the house, just in case. We were hopeful that he was just far enough away in the open-air dugout that he avoided contracting COVID-19. Six of the sixteen 16 boys on the team tested positive, including Carson.
He had a mild case. We isolated him in his room for the first few days, and he carried disinfecting wipes to wipe down the door handles and faucets he touched. He never had a fever, and his worst symptoms were that he lost taste and smell. We actually made light of that, having him taste things he would never eat, like super spicy Aardvark Habanero sauce. He didn’t even blink! We thought he was one of the lucky ones who would just recover and have immunity.
On August 4, Carson pitched in a baseball game. He came home and told us that he had experienced some super weird and uncomfortable symptoms. His heart had started “pounding and fluttering” and he said he felt light-headed, like he might pass out. I had read about the high incidence of myocarditis in college athletes post-COVID, and was concerned that his symptoms sounded similar. I called a sports medicine doctor that we had previously worked with, but he did not have any experience with post-COVID symptoms, and he referred us to a cardiologist. The heart clinic was hesitant to take him because he was a minor, so it took a couple of weeks to find a doctor who would evaluate him, then we had to wait four weeks for the initial appointment.
In the meantime, Carson was having heart arrhythmias and light-headed feelings a couple of times a week, especially when he was being active. It was hard to know what to do! He had immunity, so he was actually more “free” to do things, but I was concerned that even a ball game with his friends at the park could cause his heart to beat irregularly. He also started showing other symptoms of inflammation: chronic fatigue, insomnia, night sweats. The kid who never napped suddenly needed one every day.
Finally, we were able to see the cardiologist in mid-September. He said the symptoms sounded concerning but Carson would need several tests to confirm a diagnosis. In the meantime, he said Carson could continue normal activities, but to stop if he felt any flutters. It took another six weeks to get results from the EKG and echocardiogram plus lab work, and they ended up being somewhat inconclusive. So, the doctor ordered an MRI of Carson’s heart in mid-November. The day following the MRI, the office called at and asked if we could do a virtual visit with the cardiologist immediately. My heart dropped. Carson’s comment when I told him was “Damn. I feel like they are going to tell me I’m about to drop dead.”
Carson was officially diagnosed with viral myocarditis on November 16, over four months after “recovering” from COVID-19. There is no treatment aside from time and rest. The cardiologist helped him find his max heart rate and advised him not to go over 60% of that max rate for the next three months. He explained that pushing an inflamed heart could result in dangerous arrhythmias and would delay healing. He will have a stress test and begin to evaluate healing progress in February. There are a lot of people walking around with unknown post-COVID inflammation, including myocarditis. If they elevate their heart rate, they could have an arrhythmia that stops their heart. I worry about the kids on the baseball team who also had it but haven’t shown any reason to check for inflammation.
For Carson, 120 beats per minute is 60% of max. He put on a heart rate monitor and began testing what he could do within that limit. Jumping rope? Nope. Riding a stationary bike? Nope. Walking on an elliptical? Nope. Lifting weights? Only if they were light. A completely healthy, teenage athlete is now limited to walking, light weights and stretching. He has to be thoughtful about even goofing around with a friend, making sure his heart doesn’t beat too fast. It is frustrating and depressing. Due to his inflammation levels his pediatrician advised postponing his regularly scheduled vaccines, so he is less protected against other viruses while he heals. Even if the vaccine is widely available and Oregon high school sports resume, his upcoming senior baseball season is in jeopardy and his dreams of college baseball are dwindling.
Our experience with COVID-19 is one I don’t think many people consider. The widespread thought is that patients either are asymptomatic/have mild symptoms and recover, or they are so sick that they are in the hospital. There is a growing population of COVID-19 “long haulers” – people who survived the infection but are living with symptoms that change the way they live their lives. Carson doesn’t have a recovery timeline, and the long-term prognosis is unknown. There isn’t enough post-COVID myocarditis recovery information out there to find things we can do to “help” his body fight this inflammation. All of the unknowns feel very overwhelming, and seeing the lack of concern other people have for this virus is upsetting. We knew the seriousness, we took all the precautions until July 7, and now we have to live with the repercussions of our calculated risk.
The best way to prevent long-term health effects of COVID-19 is to prevent exposure to the coronavirus that causes COVID-19. Do not let your guard down and continue to practice social distancing, hand hygiene and mask wearing. When a safe and effective vaccine against COVID-19 becomes available make it a priority to get vaccinated. You can learn more at Lung.org/covid-19.
Disclaimer: The information in this article was medically reviewed and accurate at the time of posting. Because knowledge and understanding of COVID-19 is constantly evolving, data or insights may have changed. The most recent posts are listed on the EACH Breath blog landing page. You may also visit our COVID-19 section for updated disease information and contact our Lung HelpLine at 1-800-LUNGUSA for COVID-19 questions.
Blog last updated: June 7, 2024